Racial disparities for COVID19 mortality in Georgia: Spatial analysis by age based on excess deaths
Abstract
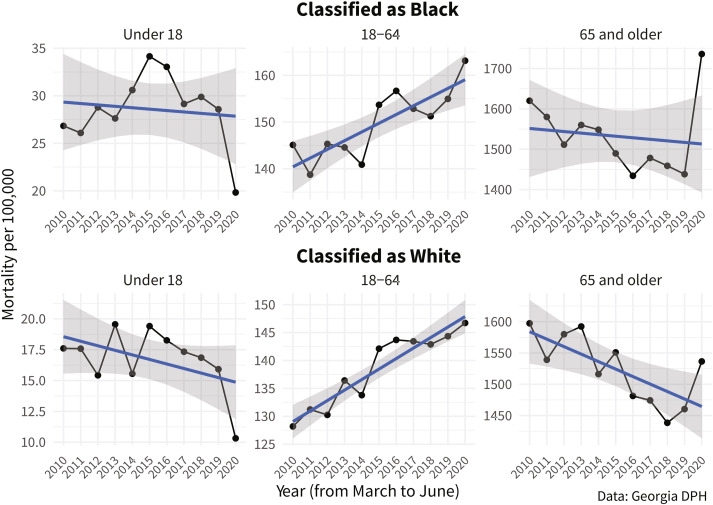
This study uses multiple measures of excess deaths to analyze racial disparities in COVID-19 mortality across Georgia. The Georgia Department of Public Health provided monthly mortality data for 2010–2020 stratified by race/ethnicity, age, county, and recorded cause of death. We first calculate crude mortality rates by health district during the time period for all groups for March through June for our historical period to identify significant time-series outliers in 2020 distinguishable from general trend variations. We then calculate the mean and standard deviation of mortality rates by age and racial subgroup to create historic confidence intervals that contextualize rates in 2020. Lastly, we use risk ratios to identify disparities in mortality between Black and White mortality rates both in the 2010–2019 period and in 2020. Time-series analysis identified three health districts with significant increases in mortality in 2020, located in metro Atlanta and Southwest Georgia. Mortality rates decreased sharply in 2020 for children in both racial categories in all sections of the state, but rose in a majority of districts for both categories in adult and older populations. Risk ratios also increased significantly in 2020 for children and older populations, showing rising disparities in mortality during the pandemic even as crude mortality rates declined for children classified as Black. Increased mortality during the COVID-19 outbreak disproportionately affected African-Americans, possibly due, in part, to pre-existing disparities prior to the pandemic linked to social determinants of health. The pandemic deepened these disparities, perhaps due to unequal resources to effectively shelter-in-place or access medical care. Future research may identify local factors underlying geographically heterogenous differences in mortality rates to inform future policy interventions.